If your body’s sounding the alarm, don’t hit snooze. An ER physician breaks down the pains you need to take seriously—no self-diagnosing in the group chat allowed.
We’ve all done it—felt a weird twinge, Googled it at 2:14 AM, and somehow landed on a diagnosis that involves rare jungle parasites or impending doom. But there’s a difference between being body-aware and being a chronic WebMD warrior. Sometimes, your body is trying to really tell you something—and ignoring it could cost you more than just a co-pay.
That’s why we tapped into the wisdom of ER physicians (you know, the people who deal with literal life-or-death decisions between sips of bad hospital coffee). One physician laid it all the way out—here are five types of pain that should stop you in your tracks and get you to urgent care or the ER faster than you can say, “It’s probably just gas.”
1. Chest Pain (Because Yes, It Could Be Your Heart)
Let’s start with the heavy hitter: chest pain. It’s not always a heart attack, but when it is? Time is everything.

What it could mean: Heart attack, blood clot, collapsed lung, acid reflux (if you’re lucky).
Why it’s urgent: Especially if it comes with shortness of breath, dizziness, or pain radiating down your arm—this isn’t the time to “wait and see.” Women, especially Black women, are often misdiagnosed or dismissed in cardiac events. Don’t let internalized “be strong” culture be your downfall.
When to go: Immediately. Call 911 if it feels crushing, like an elephant is tap dancing on your sternum. [American Heart Association]
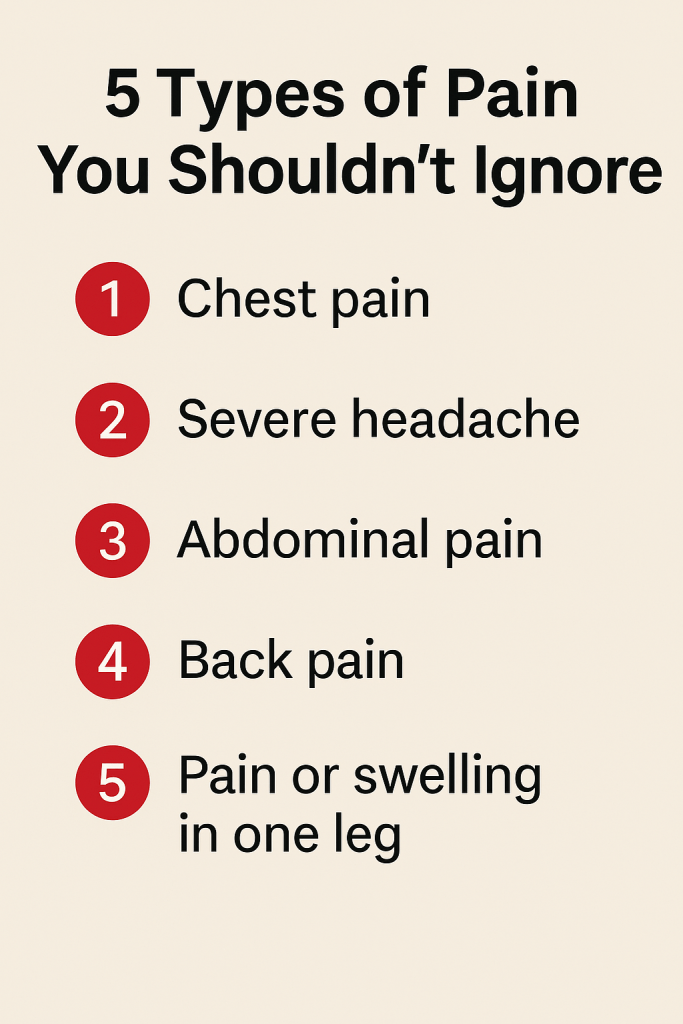
2. Abdominal Pain That Comes Out of Nowhere
Not all belly pain is burrito-related. If it’s sudden, severe, or unlike anything you’ve felt before, get checked.
What it could mean: Appendicitis, gallstones, ectopic pregnancy, ovarian torsion (yep, that’s a thing), or even a bowel obstruction.
Why it’s urgent: ER docs see people roll in doubled over way too late. By then, it’s surgery-or-else territory.
When to go: If it comes on fast and furious (not the movie), is on the lower right side, or you’re also vomiting and can’t keep fluids down—slide out the group chat and into the ER. [Insert link to Mayo Clinic abdominal pain guide]
Bonus tip: Period pain can be brutal, but if it feels “wrong,” sharp, or one-sided, don’t dismiss it. Your ovaries could be throwing hands.
3. Headaches That Aren’t Playing Fair
Not every headache is just dehydration or screen-time overload.

What it could mean: Aneurysm, stroke, or meningitis. Yes, it’s rare—but “worst headache of your life” is an actual red flag phrase ER docs listen for.
Why it’s urgent: A thunderclap headache (sudden and severe) or one that comes with neck stiffness, fever, vision issues, or confusion needs medical attention. Stat.
When to go: If it’s the worst headache you’ve ever had and it hit like a bolt out of nowhere, don’t grab Tylenol—grab your keys or call a ride. [Signs and Symptoms of Stroke]
4. Severe Back Pain (Especially With Numbness or Loss of Bladder Control)
Listen. If your back is screaming and your legs or toes go numb? That’s not “I slept wrong.” That’s a 911 call waiting to happen.
What it could mean: Herniated disc pressing on nerves, spinal cord issues, or even an abdominal aortic aneurysm (rare but real, especially if you smoke or have high blood pressure).
Why it’s urgent: If your spine is involved, delay can lead to permanent damage.
When to go: If the pain is sharp, disabling, or comes with numbness, weakness, or bathroom accidents—you don’t need a second opinion. You need an ER.
5. Leg Pain That’s Not Just “From the Gym”
Soreness after leg day is one thing. A hot, swollen, tender calf? Whole different story.
What it could mean: Deep vein thrombosis (DVT), aka a blood clot, which can break off and cause a pulmonary embolism—a potentially fatal blockage in your lungs.
Why it’s urgent: Black women are often under-screened for DVT despite having higher risk factors, including higher rates of obesity, pregnancy complications, and sickle cell traits. Don’t downplay it.
When to go: If one leg is visibly larger than the other, redder, and hurts more than it should, stop blaming leg day. [About Venous Thromboembolism (Blood Clots)]
The Takeaway: Pain Is Communication, Not a Weakness
If there’s one thing ER doctors want us to unlearn, it’s the idea that pushing through pain is some badge of honor. That mindset is outdated, dangerous, and frankly, exhausting.
Black women especially are conditioned to be “strong,” to not make a fuss, to dismiss symptoms because we’ve been dismissed by healthcare systems for generations. But strength also looks like advocating for yourself—like walking into an ER and saying, “I’m not okay, and I need someone to take this seriously.”





Leave a comment