It’s Not “Just a Headache.” Let’s Get Real About Why This Common Affliction Remains One of Medicine’s Greatest Mysteries—and What We Can Do About It.
We’ve all been there. That dull throb that starts behind your eyes after a marathon session of doomscrolling or that sharp, pulsing pain that hits out of nowhere, making you question your entire existence. For most, it’s a nuisance, a temporary glitch in the system. Pop a couple of ibuprofen, down a bottle of water, and move on.
But what about when the headache is your unwelcome roommate, dictating your entire life? For millions of us, chronic headaches—from debilitating migraines to terrifying cluster headaches—aren’t just an inconvenience; they’re a permanent resident in our skulls who doesn’t pay rent.
So, here’s the burning question: In a world where we’re talking about A.I. that can write poetry and medical science is developing personalized cancer treatments, why the hell hasn’t anyone found a cure for this? Why are we, as intelligent, ambitious, and multifaceted women, still having to explain to people that it’s not “just a headache”?
It’s a brilliant, brilliant question. And the answer is complex, infuriating, and, honestly, kinda messed up.
The Big Problem: It’s All in Your Head (And That’s the Point)
The reason medical science has been slow on the draw is rooted in a long, complicated history of dismissal. For centuries, headaches have been treated as a trivial, psychological, or even hysterical condition, particularly when it affects women. This isn’t some conspiracy theory; it’s a documented, frustrating reality. As journalist Tom Zeller Jr. explores in his book, The Headache: The Science of a Most Confounding Affliction—and a Search for Relief, the medical community has, for a long time, considered headache disorders “a trivial choice for specialization.”
Because of this historical neglect, research has been historically underfunded and under-prioritized. Think about it: diseases with a clear, visible physical marker—a tumor, a broken bone—get the big bucks and the top minds. But a condition whose primary symptom is invisible pain, which can’t be seen on an MRI or a lab test, often gets the side-eye. You know that feeling when you go to the doctor and you just know they think you’re exaggerating? That’s been the collective experience for headache sufferers for generations.
And let’s be real, a huge part of the problem is that so many women—a demographic that has been historically ignored in medical research—suffer from these conditions. Research has shown that gender bias in medicine is real, and it has played a role in how chronic pain, particularly migraines, has been diagnosed and treated (or not treated) over the years. We were told to “power through it” or that it was “just stress” or “hormones,” when what we were actually experiencing was a complex neurological condition.
A Confounding Chaos of Causes
Another major reason for the lack of a “cure” is that headaches aren’t a single, uniform thing. They are a wildly diverse group of conditions, each with different triggers and mechanisms. It’s like trying to find a single key that opens every single lock in the world.
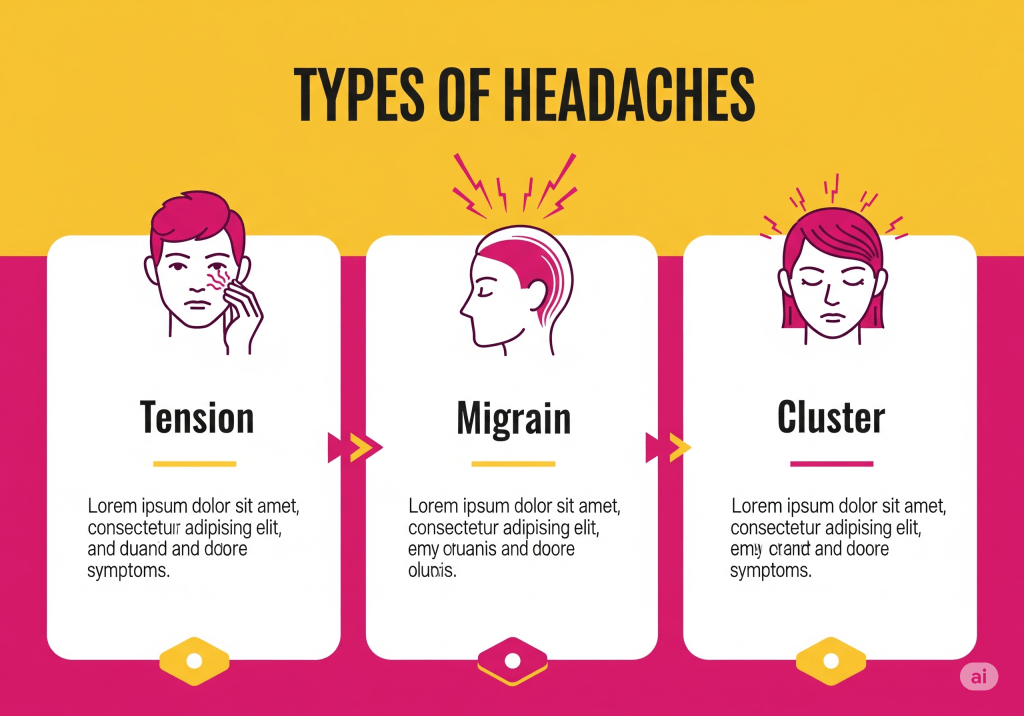
- Tension Headaches: Often caused by mental or physical strain, lack of sleep, or muscle tension.
- Migraines: A complex neurological disease with symptoms that go far beyond head pain. These can include auras, extreme sensitivity to light and sound, nausea, and vomiting.
- Cluster Headaches: Described as one of the most painful conditions a human can endure, often featuring intense, excruciating pain that strikes in “clusters.”
The triggers for these can be a chaotic mix of genetics, environmental factors, and lifestyle. Things like dehydration, specific foods, weather changes, or even too much caffeine can flip the switch. It’s not a one-size-fits-all problem, which makes finding a single cure a monumental task. The approach has to be as varied as the causes themselves.

The Hopeful Horizon: Progress, Not Perfection
Okay, so we’ve established that the medical field has been sleeping on us. But it’s not all doom and gloom. The good news is that things are finally starting to change, and we’re seeing more progress in the last five to ten years than in the previous three decades.
We are entering a new era of understanding. Researchers are delving deeper into the neurological pathways that cause pain. A major breakthrough has been the discovery and development of CGRP (calcitonin gene-related peptide) inhibitors. These are a new class of drugs designed specifically to target the protein that plays a key role in triggering migraines. They aren’t a cure, but for many, they are a game-changer, reducing the frequency and severity of attacks.
Beyond medication, there’s a growing appreciation for a holistic approach. This includes:
- Lifestyle Adjustments: Identifying your personal triggers and making strategic changes to your diet, sleep, and stress management.
- Mindfulness & Biofeedback: Learning to recognize and control bodily responses to pain.
- Alternative Therapies: From acupuncture to massage, people are finding relief in practices that help manage pain and stress.
This shift acknowledges what we’ve always known: managing chronic headaches requires a multifaceted strategy. It’s not just about popping a pill; it’s about paying attention to our bodies, advocating for ourselves with doctors, and building a toolkit of both traditional and alternative methods that work for us.
“If there’s a lesson here, it’s that pain resists mastery, but understanding, however incomplete, can offer its own form of relief.” — The New Yorker
The Takeaway
So, has medical science cured chronic headaches? No. Not yet. But we are finally, collectively, having an honest conversation about the reality of chronic pain. We are pushing for better research, demanding more specialized care, and refusing to be dismissed. The future isn’t about finding a single magic bullet. It’s about empowering ourselves with knowledge, finding our own fierce-and-fun-but-also-take-it-seriously wellness strategies, and building a world where no one has to suffer in silence because their pain is “invisible.”
This isn’t a plea for pity. This is a call to action. We have to be our own brilliant advocates, and in doing so, we not only heal ourselves but also help reshape a medical system that has historically failed us.
Because it’s not “just a headache.” It’s a complex, challenging, and all-too-common part of our lives, and it’s time we finally talked about it with the honesty and brilliance it deserves.
Links/References:
- General information on headache and migraine: The National Institute of Neurological Disorders and Stroke
- A look at the historical dismissal of women’s pain: Gaslighting in women’s health: No, it’s not just in your head





Leave a comment