Prostate screening isn’t just “his” issue—it’s everyone’s conversation. Time to get real about the pros, the cons, and why it matters.
Alright, Millennial sisters and fierce femmes, let’s talk about something that isn’t usually on the menu—but definitely should be: prostate cancer screening. I know—it’s not our body part, but hold up. This silent epidemic needs unsilencing, and yes, it affects us, too—professionally, emotionally, societally. So here’s your honest, bold, brilliant breakdown: what works about PSA testing and what might not. Spoiler alert: the truth is nuanced, and that’s where the power lies.
Why Everyone Should Care
Prostate cancer is the second leading cause of cancer death in men in the U.S., even though it usually progresses slowly—and quietly . Many men have no symptoms until it’s advanced . That makes early detection a potential lifeline—but also a muddled pathway, packed with pitfalls.
The PSA Test—Pros
- Can save lives. PSA screening may prevent approximately 3 deaths per 1,000 men screened. Some argue the benefit is even greater—up to 10 lives in 1,000—depending on study and methodology.
- Early detection matters. Finding aggressive tumors before they metastasize can dramatically improve outcomes.
- Informed choice is power. Organizations like the CDC encourage conversations with doctors about personal risk and values—not blanket “yes/no” decisions.

The PSA Test—Cons
- Overdiagnosis and overtreatment. Up to 60 out of 1,000 men diagnosed via PSA screening may have cancers that would never have caused harm—but treatment brings real side effects.
- Harsh side effects. Treatment—especially surgery or radiation—can lead to incontinence and erectile dysfunction.
- False alarms. PSA levels can be elevated due to benign conditions like BPH or infection, triggering anxiety and unnecessary biopsies.
- False reassurances. Normal PSA doesn’t guarantee you’re cancer-free—some cancers evade detection.
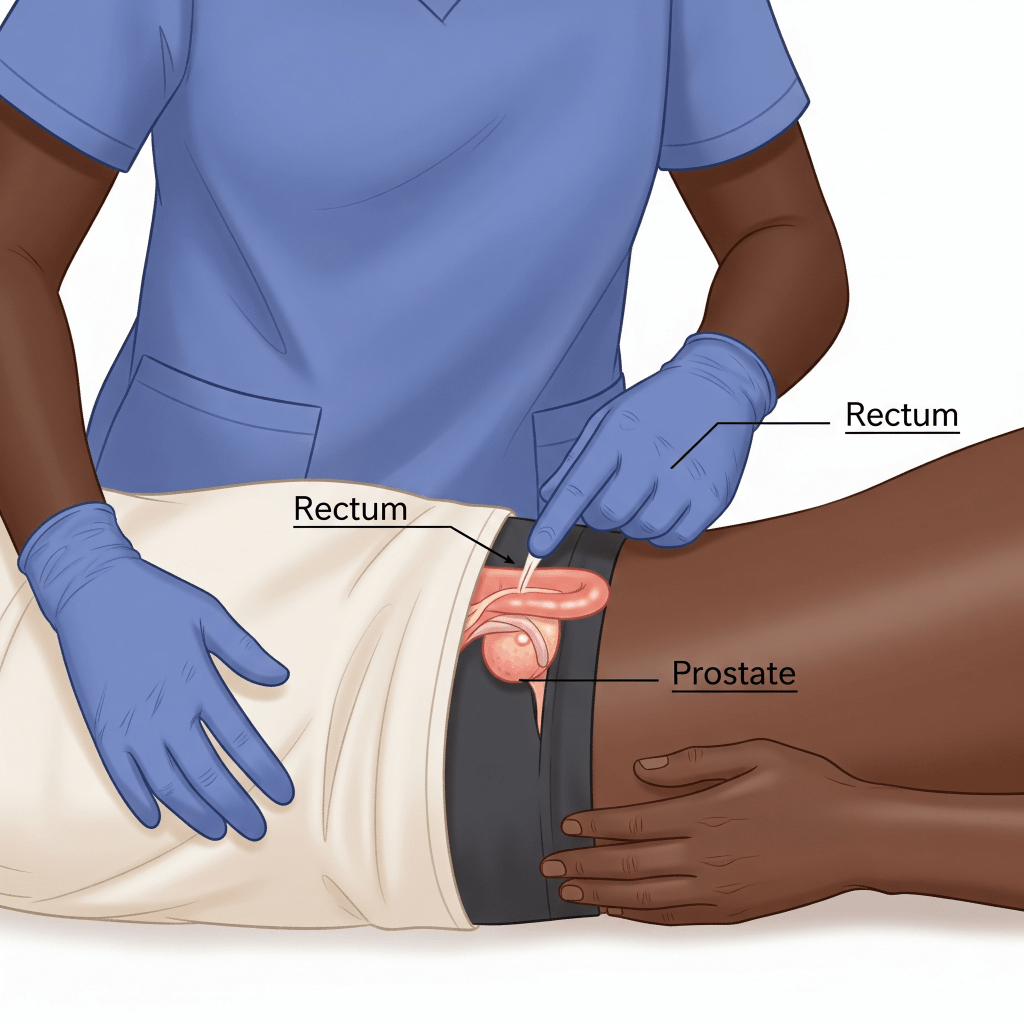
DRE (Digital Rectal Exam)—Does It Even Help?
In short: not really. Major health bodies, including the USPSTF, advise against using DRE alone for screening—it hasn’t proven to reduce mortality and offers little added value.
Modern Moves: Smarter Screening
- MRI-guided biopsies and AI. New tools like MRI targeting (and even AI-assisted imaging) improve accuracy and reduce unnecessary biopsies.
- At-home saliva tests. Emerging research suggests these gentle spit tests may better predict genetic risk than traditional blood tests.
When Screening Makes Sense
- High-risk groups: Black men and those with family history face greater risks and should consider earlier, informed conversations.
- Age 55–69: The sweet spot—many guidelines recommend PSA decisions made with a clinician, balancing pros and cons.
- Over 70? Screening is generally not recommended for healthy older men—it may cause more harm than good.
- Symptomatic? If urinary issues or pain arise, it’s definitely time to check—not a moment to wait .
Real Stories, Real Stakes
The Oscar-winning director (no, not the 1970s one, but the modern-day visionary) turned his defeat—and grief—into a call for justice. After losing his father and friend Alex Wheatle to prostate cancer, McQueen’s own early-stage diagnosis ignited his mission. He now advocates for targeted screening and better communication within Black male communities, exposing systemic bias and health inequities.
A longtime civil-rights icon and co-founder of The Freedom Singers, Neblett transformed his Stage IV diagnosis into a social movement. Launching the #BlackProstateCheckChallenge, he’s pushing for awareness campaigns, health equity, and even creating a National Black Prostate Cancer Week—with help from his family and public figures like Anthony Anderson. His initiative has already touched 67 million people.
Super Bowl champ, NFL legend—and prostate cancer survivor. Diagnosed in 2016, Sharpe shared how a family history spurred regular screening in his 30s. Opting for a less invasive treatment, he’s now in remission and openly encourages Black men to prioritize early detection.
A 47-year-old Chicago artist and Northwestern Medicine employee, Jones had zero symptoms—yet his doctor’s proactive suggestion for a screening changed his life. Elevated PSA → MRI → biopsy → robotic prostatectomy—and he’s cancer-free. Now, he channels that relief into awareness work, especially for Black men.
A Harlem political powerhouse and VP at Fresh Direct, Blackmon’s wake-up call came after actor Chadwick Boseman’s untimely passing. His PSA was high during a routine check—leading to an MRI, biopsy, and ultimately, treatment. He’s now a fierce advocate, sharing his story widely and encouraging Black men to talk to their doctors.
Why These Stories Matter
These aren’t just “other men’s” stories—they reflect the urgency, diversity, and depth of real Black experiences with prostate cancer. From activists to athletes, artists to powerbrokers, these narratives break stigma, build dialogue, and spotlight how early detection can reshape lives.

Our Feminist Millennial Takeaway
Here’s the takeaway for us: the word “prevention” isn’t just a boring medical box to check—it’s an invitation to shape health outcomes, not just for ourselves but for the men in our lives. Engage openly. Encourage informed dialogue. Demand smarter, more equitable screening protocols that account for race, age, and autonomy.
Links & References
- Guardian feature: The silent epidemic: the pros and cons of screening for prostate cancer
- CDC guidance on screening choices
- PSA benefit vs harm analysis (NCBI)
- Modern MRI/AI diagnostic pathways
- At-home saliva test findings
- Risk in Black/African-American communities PSA and DRE guidelines (USPSTF, Hopkins, etc.)




Leave a reply to The Fierce Guide to Ghost Pain: Why Your Brain is the Real MVP of Pain Management – Fierce Millenial Cancel reply